Pre-Pandemic Timeline – 1800s
Chronological order of significant data points
that have helped to shape our world.
Navigate the timeline pages:
You Are Here | 1900-1945 | 1946-1979 | 1980-1999 | 2000-2015 | 2016-2018 | 2019 | 2020 | 2021 | 2022 | 2023
Best viewed on a large screen
Data points are continuously being added so please come back again soon.

Edward Jenner experiments with cowpox pus to inoculate against smallpox
The US Vaccine Act of 1813 – first consumer protection legislation
The Vaccine Act of 1813 was an Act of the Twelfth Congress of the United States to encourage vaccination against smallpox. It was passed February 27, 1813. On the back of a 1821 outbreak of smallpox in North Carolina, the act was repealed May 4, 1822 handing the authority to regulate vaccines back to the states. This Act was the first federal law in America concerning consumer protection and pharmaceuticals. [1, 2]
Congress of Vienna
From September 1814 to June 9, 1815 the Congress of Vienna, a series of international diplomatic meetings to discuss and agree upon a possible new layout of the European political and constitutional order and negotiate”a long-term peace plan for Europe by settling critical issues arising from the French Revolutionary Wars and the Napoleonic Wars”, after the defeat and surrunder of French Emperor Napoleon Bonaparte in May 1814. Participants were representatives of all European powers and other stakeholders, chaired by Austrian statesman Klemens von Metternich. [1, 2]
The Congress’s agreement was signed June 9, 1815 , just 9 days before Napoleon’s final defeat at the Battle of Waterloo on June 18, 1815.
“Some historians have criticised the outcomes of the Congress for causing the subsequent suppression of national, democratic, and liberal movements, and it has been seen as a reactionary settlement for the benefit of traditional monarchs. Others have praised the Congress for protecting Europe from large and widespread wars for almost a century.” [1]
Oldest US hospital, Bellevue, opens it’s new doors
In 1811 the city of New York purchases Kips Bay farm and constructs a new almshouse, which becomes known as the Bellevue Establishment, the hospital facility opens on April 29, 1816. Two years later in 1818 it is the first hospital that requires a qualified physician to pronounce death. [1]
Bellevue Hospital lays claim to being the oldest hospital in the US as it traces back to March 31, 1736, when on the present site of City Hall, the Almshouse Hospital was established. It started as the “Publick Workhouse and House of Correction of the City of New York”.
Dutch immigrant, Dr. Johannes van Beuren, “through the influence of the governor of the colony” was appointed as the first physician, he stayed there until his death in 1755. His son Dr Beekman van Beuren who took over in 1765 until 1776, “is credited with the introduction of inoculation for smallpox in the public institutions of the city”. van Beuran’s are ancestors to the 8th President the of the U.S.
In 1825 “Bellevue Hospital” officially gets it’s name by the Common Council of NYC. “In a medical staff reorganization, the office of visiting physician is abolished, and the position of ‘resident’ physician is created”. In 1847, the hospital is separated from the Almshouse Authority. A board of visiting physicians and surgeons takes charge and a permanent Medical Board is created, a medical and a surgical division are also formed. This happens the same year the American Medical Association is established.
On March 2, 1849 the operating theatre and clinical lecture room of the hospital was formally opened and “dedicated to the united interests of science and humanity”. That day in the amphitheatre, to “give a practical illustration” of the teaching facility, Dr. William van Beuren performed a the first public clinic, performing a “lithotomy” (removal of bladder stone) on a 67 year old man who was anaesthetised by chloroform and ether. Eight days later “Dr. Van Buren ampulated the arm of a man whose wrist and hand had been rendered useless, and a source of constant irritation by phlegmonous erysipelas” a bacterial inflammation, so they cut it off and solved the problem! [2]
Bellevue claims many medical historical firsts, one being the recipient of Andrew Carnegie’s, first public gift of $50,000 in 1884. Carnegie’s Foundation funded The Flexner Report!
First US College of Pharmacy is established – setting up the framework for drug control
In 1816 the Trustees of the University of Pennsylvania established a Faculty of Natural Sciences, and “Dr. James Mease was granted permission to open a regular course of lectures on pharmacy” which he had done for 2-3 years. By 1819 “the Board of Trustees resolved that the teaching of the pharmaceutical art should be a part of the duties of the professor of materia medica and pharmacy, and that a course of lectures be established intended for pharmaceutical students”.
Following a proposal by Dr. John Redman Coxe, a medical school professor of chemistry, on February 6, 1821 the University Trustees passed a resolution to institute a Degree of Master of Pharmacy, from this the Philadelphia College of Pharmacy was established, the first of it’s kind. [1] After meeting with the druggists and apothecaries who were concerned this change would “diminish the number of apothecaries, and the profits of those who remained would be increased”. [2]
In 1817 Dr. Lyman Spalding submitted a proposal to a NY Medical Society for a national work to be prepared and published by the medical societies and schools of the United State, from this the Pharmacopoeia 1820 was eventually established.
On March 27, 1821 the Trustees held their first meeting and elected the board of trustees for School of Pharmacy. Local philanthropist Daniel B. Smith was elected secretary, he would play a large role in the college.
On March 31, 1848 the Philadelphia College of Pharmacy adopted that a Code of Ethics be established.
“Pharmacy being a profession which demands knowledge, skill and integrity on the part of those engaged in it, and being associated with the medical profession in the responsible duties of preserving the public health, and dispensing the useful though often dangerous agents adapted to the cure of disease, its members should be united on some general principles to be observed in their several relations to each other, to the medical profession, and to the public.”
In December 1825 the Journal of the Philadelphia College of Pharmacy began to publish the advances in the pharmaceutical sciences.
The New York College of Pharmacy was established in 1829 in the heart of where imported drugs came into the country. They were active in getting the Import Drugs Act 1848 passed, to prevent the shipment of adulterated drugs and chemicals into the country. This helped protect the quality of the drug prescribed by the allopathic physician.
“In 1900 this code of ethics was somewhat modified to meet the modern conditions of pharmaceutical practice”, as was the medical code of ethics around the same time.
Philadelphia is the home of Pharmacy in the US and a city with an alarming death spike in the 1918 pandemic!
Homeopathy begins in England, becomes popular after cures Queen Adelaide
“In 1830, homoeopathy was introduced in England by the noble family of Shrewsbury, who had become acquainted with it during their travels on the Continent. Soon after Lady Shrewsbury was married to the Italian prince, Doria Pamphili, who was followed to England by his body physician, the homoeopath Dr. De Romano. He opened a clinique on the family estate ” Alton Tower,” in Derbyshire, and was assisted by Drs. Daniellsand Roch.
In February, 1830, they were mentioned — not in the most Mattering terms — by the British and Foreign Review, (Forbes) but in 1839 that Journal had very much changed its tone, because meantime, the Queen Dowager Adelaide, after having been given up by her allopathic physicians, was saved… by Dr. Stapf, [Johann Ernst Stapf] an eminent homeopathic physician in Naumburg, who had been expressly sent for to Germany [in 1835]. This cure opened the mansions of nobility to the new system, and gained many friends for it.” Wikipedea makes no mention of this “cure”. [1, 2]
Dr. Frederick Hervey Foster Quin (1799-1878) physician to King Leopold of Belgium, set up practice in London in 1832 and was the Founder and President of the British Homoeopathic Society in 1844 and in October 1849 he founded The London Homoeopathic Hospital (later The Royal London). Quin is said to have introduced Homeopathy to England late 1820s. [3]
Homeopathy has been popular amongst England’s royalty, including late Queen Elizabeth II and now King Charles III, who in 2019 became patron, which caused an uproar.
Home of the BMJ is founded
On July 19, 1832 Sir Charles Hasting’s founded the Provincial Medical and Surgical Association (PMSA) which published a weekly medical journal. By 1856 they became the British Medical Association (BMA) known today as a registered trade union for doctors in the United Kingdom. [1]
The Provincial Medical and Surgical Journal which began Oct 3, 1840 (which happened to mention smallpox vaccination, an act performed by surgeons!), merged with the Association Medical Journal in 1857 to become the British Medical Journal (BMJ). [2]
The BMA Medical Reform Committee after 20 years of negotiation successfully drafted and secured the passing of the Medical Act 1858, which established the General Medical Council and the Medical Register, therefore distinguishing, for the first time, between the qualified and unqualified practitioners – on their terms. “This also positioned the BMA to play a major role in future medical politics, campaigning on issues such as Poor Law Medicine, quackery, public health, alternative medicines and military medicine, and contract practice. During this time one of the most active and influential of the association’s bodies was the Parliamentary Bills Committee, formed in 1863 to take a leading role in influencing legislation on public health matters” [1, 2]
US national debt $0 for first time in history
By January 8, 1835 the United States national debt reaches $zero for the first time in history, after President Andrew Jackson, keeping his promise pays off remaining debt to the private central bankers. [1]
The British bankers respond in retaliation, causing the financial crisis called the “Panic of 1837“, and Jackson gets blamed!
- The next government bail-out happens in 1907 by JP Morgan, America’s “informal central banker, in the absence of a central bank,” a crisis he created, which leads to the creation of the Federal Reserve Act in 1913.
First homeopathic medical school opens in the United States
Opened April 10, 1835 by several prominent homeopathic physicians, Allentown Academy of Homoeopathy was the first homeopathic medical school in the United States and the world. It educated the first generation of American homeopaths that would go on to bring homeopathy to new heights in the country. [1, 2, 3, 5]
The Academy flourished until 1843 when it was discovered that its treasurer, Allentown banker John Rice, had embezzled the school’s funds. It then moved to Philadelphia and developed into the Hahnemann Hospital. [4]
America’s first national medical society was established
“Homeopathy began growing in the New World shortly after Dr Johannis Gram, a Dutch homeopath, emigrated to the United States in 1825. It expanded so rapidly that the homeopaths decided to create a national medical society.” [1, 2] Or was it Danish physician Hans Burch Gram who settled in Boston, New York in 1828! [4]
On April 10, 1844 the American Institute of Homeopathy was formed, thus becoming America’s first national medical society, and was seen as a threat by Allopathic medical men. This day marks the birthday of the founder of homoeopathy, Samuel Hahnemann, a year after his passing.
At the time homeopathy was popular among the “educated and upper classes,” and some hospitals and insane asylums were exclusively ran by homeopaths, most often curing those that allopathic practitioners deemed “incurable“. Homeopathy was a “significant competitor” to orthodox/allopathic medicine, which at the time still used ‘barbaric’ treatment techniques such as blood letting and use of leeches along with medicines containing toxic mercury, lead, and arsenic! [3]
The allopathic practitioners tried to attribute homeopathic success [9] to the “over-dosing of patients by the ordinary practice” [?] or “the imaginations of a susceptible class of patients” (the placebo effect), even though the evidence did not concur!
Three years later, on May 7, 1847 orthodox medicine followed suit and organised to formed the American Medical Association with the purpose of reforming medical training and establishing a code of ethics, and in turn systematically eliminated their competition!
Each organisation referred to each other as quacks! They did not get along. [5]
Have we “lost” the art of homeopathy? Was it ahead of its time, that only quantum physics could explain?
Semmelweis proposed doctors wash hands!
In 1846, Ignaz Phillipp Semmelweis, a Hungarian doctor working as the assistant of the obstetric clinic in Vienna’s General Hospital, investigated why women giving birth in a hospital maternity ward staffed by all male doctors and medical students had a 5 times higher death rate due to “childbed fever” than women who gave birth in a hospital staffed by female midwives. [1]
Following the death of a male friend, punctured by a scalpel and dying of the same “childbed fever”, in 1847 Semmelweis proposed the practice of washing hands with chlorinated lime solutions between going from conducting autopsy’s to then delivering babies! Under his measures the mortality rate averaged only 0.85% compared to 10-15% under ‘normal’ practice. [2, 3]
Semmelweis’s observations conflicted and were rejected by the established medical authority. Though the Hungarian government adopted his “prophylactic practice” in 1855. By 1861 his mental health declined into depression, leading to his committment to an asylum in 1865, where he was beaten, became infected and died 2 weeks later on August 13, 1865 likely of sepsis. [3]
The founding of “antiseptic medicine” was credited to surgeon Sir Joseph Lister, not Semmelweis! “In 1864, while working at Glasgow University as Professor of Surgery, Lister was introduced to Pasteur’s germ theory of disease, and decided to apply it to the problem of surgical infections.” [4]
The American Medical Association is formed
At the February 1845 New York State Medical Society meeting, Dr Nathan Smith Davis “earnestly” recommend that a National Convention of Delegates from Medical Societies and Colleges in the whole Union… convene in the city of New York on the first Thursday in May, in the year 1846…”, the purpose begin to form a national medical association to “raise standards of medical education and of medical ethics”.
At this time medical school was “not exactly rigorous” nor costly. Dr Nathan Smith Davis (N.S.D) wrote about the sub-standard education in the Nov 1845 volume of the NY Journal of Medicine (NYJM) dated Sept. 22, 1845:
“All the young man has to do is gain admittance in the office of some physician, where he can have access to a series of ordinary medical text-books, and see a patient perhaps once a month, with perhaps a hasty post-mortem examination once a year; and in the course of three years thus spent, one or two courses of lectures in the medical colleges, where the whole science of medicine, including anatomy, physiology, chemistry, materia medica, pathology, practice of medicine, medical jurisprudence, surgery, and midwivery are all crowded upon his mind in the short space of sixteen weeks…and his education, both primary and medical, is deemed complete.” [1, 2]
The following year at the May 5, 1846 convention, Dr Davis was elected “chairman of the Committee on Correspondence relative to Medical Education and Examination” to summon the 1847 convention. The committee visited medical societies and colleges around the country presenting their proposal. It was because of his involvement Davis became known as the Founder of the AMA.
On May 7, 1847, at The Academy of Natural Sciences in Philadelphia, Pennsylvania, the National Medical Convention was held, attended by “250 delegates representing more than 40 medical societies and 28 colleges”. The delegates “approved a resolution to establish the American Medical Association (AMA) and elect Dr. Nathaniel Chapman as its first president.” [3, 4]
The AMA aimed to “establish both uniform educational requirements and a medical code of ethics” [8], which in 1903 became The Principles of Medical Ethics. [5, 6] They deemed homeopathy as “quack remedies” which at the time were “flourishing’.
Members of the AMA “had great animosity towards homeopathy and decided to purge all local medical societies of physicians who were homeopaths” or had any association with with them. [7]
- In 1883, when Dr Davis was 66, he became the first editor of the Journal of the American Medical Association (JAMA), – the weekly periodical replaced the AMA’s yearly Transactions.
- On April 20, 1905 the AMA formed the Council on Medical Education, Ttey held 4 confernces, 1905, 1906, 1907 , and May 1908, before the Carnegie Foundation in November 1908, led by Abraham Flexner took over the task of reforming medical education in the US.
Chloroform is discovered as a human anaesthetic, replacing Ether
Scottish obstetrician, James Young Simpson, communicated to the Medico-Chirurgical Society of Edinburgh meeting on November 10, 1847 his human anaesthetising experiments using chloroform, which he published as an “Account of a New Anaesthetic Agent as a Substitute for Sulphuric Ether in Surgery and Midwifery“. Simpson and his two assistants on the evening of November 4, 1847, lost consciousness after purposely inhaling chloroform, he then used it during childbirth. Within weeks of its appearance, chloroform had almost completely replaced ether as the standard anaesthetic. [1, 2, 3, 4]
In 1867 Joseph Lister’s discovered of the “antiseptic principle“, which jointly, these discoveries opened the path for general medical surgery – “solving” the problems pain and infection. I suspect it helped spur on animal experimentation also.
Chloroform had been invented in 1831 “made by reacting acetone with chlorine”, in 1842 it was tried as an anaesthetic on animals by Dr Robert Mortimer Glover, he deemed it too dangerous for humans.
The manufacture of fine optical microscopes helps launch the Germ Theory of disease
In 1861, Pasteur published his germ theory [3]. The “Germ theory states that specific microscopic organisms are the cause of specific diseases…. The theory was developed, proved, and popularized in Europe and North America between about 1850 and 1920″, following closely the manufacture of fine optical microcopes from early 1850‘s. Microorganisms had already been discovered.
The Spencer [1, 2] microscopes were manufactured in the United States.
The first compound microscope (and telescope) is credited to Zacharias Janssen, the son of Hans Janssen, a spectacle maker from Middleburg, Holland, in the 1590s when Zach would have been a teenager. At this time eyeglasses were beginning to be popular. Though poor in image quality is a seminal advance in scientific instrumentation and discoveries. [3]
England: First complusory Vaccination Act (1853)
In 1853 “Lord Lyttelton, as a private member, brought in a bill to parliament to make vaccination compulsory in England. The bill passed through both Houses without opposition, and with hardly any debate except on points of detail”. This became the first compulsory Vaccination Act 1853. [1, 2]
Stunningly the “Act of Parliament of 1853 had no section devoted to the “Definition of Terms”; there was no definition of cowpox or genuine vaccine, an omission all the more remarkable that variolous matter was then being used as vaccine, on the pretext that it had “ passed through the cow. Although a medical dogma was therein established by the State, the doctrine was not formulated.” The Act was “simply a notorious empirical practice that was established under pains and penalties”, not of any principle of epidemiology or pathology.
“…The vaccinated are safe against smallpox because they, in fact, have had it ”
- In 1853 the Anti-Compulsory Vaccination League (ACVL) was formed in London. By 1860s a national anti-vaccination movement had formed By 1870s ACVL had 103 branches and up to 200,000 members and sympathizers in Britain alone. “Many became actively involved when their child was injured or killed by a smallpox vaccine. The present-day anti-vaccination movement is no different” [3]
The Vaccination Act of 1840 made variolation the method of inoculating with smallpox (variola), illegal. Inoculation with the same procedure but instead using cowpox (vaccinia) contaminated pus, the process called vaccination, was legal and under the Poor Law Act was administered free. [?]
U.S. Department of Agriculture is established
In December 2, 1861 an act was passed to establish the United States Department of Agriculture (USDA), President Abraham Lincoln signed the act into law May 15, 1862. Around this time half of all Americans lived on farms – which is why Lincoln referred to it as “The People’s Department.” [1, 2, 3]
The first “Commissioner of Agriculture Isaac Newton, head of the new Department of Agriculture, appointed Charles M. Wetherill to the position of Chemist of the Department in 1862, a function that the Patent Office had transferred to Agriculture.” …The position eventually grew into the Division of Chemistry and then by 1901 the Bureau of Chemistry. [5]
The role of the Division of Entomology at the USDA was to “learn everything there was to know about agricultural pests, and then to destroy them. The intended beneficiaries of this project were panicked farmers whose [emerging monoculture] fields were being decimated by insect invasions.” The first head of the USDA Division of Entomology was Charles Valentine Riley who advocated for biological control, although “amateurish” chemical compounds of “arsenic and lead and kerosene” were also sprayed over crops at the time. After Riley’s accidental death on September 14, 1895, Leland Howard, a “good progressive” took charge of the Entomology department and ushered in the era of widespread chemical pest control. [6]
Prof. Howard, who contributed to Ronald Ross’ 1910 book on Malaria, seised the opportunity to promote chemical control of insects by shifting focus to the “tormenting plague” of mosquitoes and a means of alleviating the “public health anxieties…” [6, 7]
Up until June 1940 the FDA resided under the purview of the USDA. [4] but with the advent of edible vaccines, who’s role is it to regulate prophylactic food?
The First International Organisation, the Red Cross takes shape in Geneva
The history of the Red Cross begins with an initiative of a man named Henry Dunant (from Geneva, Switzerland) who, with the help of local women, helped care for wounded soldiers at the battle of Solferino in 1859. Dunant then lobbied political leaders to take more action to protect war victims. His two main ideas were for a treaty that would oblige armies to care of all wounded soldiers and for the creation of national societies that would help the military medical services.” [1]
Dunant put down his ideas in a campaigning book, A Souvenir of Solferino, published in 1862. The Geneva Public Welfare Society formed a working group which first met in February 1863. An international conference with 16 nations convened in October 1863, to formalize the concept of national societies. National Red Cross Societies formed and the Committee of Five in Geneva eventually became the International Committee of the Red Cross (ICRC).
The standard emblem to identify medical personnel on the battlefield as agreed to be a red cross on a white background, the reverse of the Swiss flag.
On August 22, 1864, delegates from a dozen countries signed the first Geneva Convention, the founding text of contemporary international humanitarian laws, this convention made it compulsory for armies to care for all wounded soldiers, whatever side of the battle they were on.
“Dunant died in 1910. By then, in Europe, North and South America, Asia and Africa, the Red Cross and the Geneva Conventions had taken root. Both were to be put to a severe test during the First World War.” [3]
The International Federation of Red Cross and Red Crescent Societies (IFRC) was founded in 1919 in Paris in the aftermath of World War I. Originally called the League of Red Cross Societies, we were the brainchild of Henry Davison, the president of the American Red Cross War Committee. It’s mission to ” improve the health of people in countries that had suffered greatly during the war. It also sought to improve existing Red Cross Societies and promote the creation of new ones around the world.” [2]
“Within months of its creation, the League had launched a campaign to counter a massive typhus epidemic in Eastern Europe. Shortly after, it launched appeals in the wake of the Russian famine of 1921 and the Great Kanto earthquake in Japan in 1923.” And so begins the coordinatied “war on disease”.
Today Geneva, Switzerland is still the home of international organisations.
National Academy of Sciences is established
The National Academy of Sciences (NAS) [6, 7] is a private, non-profit national society of “distinguished scholars”, established March 3, 1863, spurred on by the demands of the American Civil War. The Academy serves to “investigate, examine, experiment, and report” (without personal remuneration) upon any subject of scientific and related technical problems, whenever called upon to do so by any government department. It is said to provide “independent and objective advice“. [2, 6]
The first NAS president was Alexander Dallas Bache, it was he who ” gave the most explicit and public expression of the idea of a national scientific academy”. In 1851, as outgoing AAAS president Bache “publicly recommended that the federal government establish a centralized scientific organization to be consulted by the government in matters of science and technology in order “to guide public action in reference to science matters.”
Two years later, in 1853, Bache and a group of scientists, based largely in Cambridge, Massachusetts, began meeting informally. By 1858, naturalist Louis Agassiz (who would befome the first foreign secretary), in a private letter had outlined the structure and organization of an academy of sciences. Agassiz then enlisted the support of Massachusetts Senator Henry Wilson who drafted and presented their bill for incorporation, it was passed and signed into law by President Lincoln on March 3, 1863. The organisation began with 50 charter members. [3, 4]
“Members are elected to the National Academy of Sciences in recognition of their distinguished and continuing achievements in original research. Membership is a widely accepted mark of excellence in science and is considered one of the highest honors that a scientist can receive.” There is no membership application process only already elected Academy members (control) formal nominations. [1]
Scientific and “learned” societies that were already established [5]:
- 1743 – American Philosophical Society (APS) was established in Philadelphia by Benjamin Franklin
- 1780 – American Academy of Arts and Sciences was established in Massachusetts
- 1840 – National Institute for the Promotion of Science was established in Washington
- 1846 – Smithsonian Institution was established in Washington
- 1848 – American Academy for the Advancement of Science (AAAS) were established in Philadelphia (and publishes Science Magazine)
By the 1890s the government called upon the Academy with less frequently which gave “some of the institution’s membership cause for concern”, but a “group of activist members” revitalised the institution by establishshing the National Research Council (NRC) under Academy auspices in 1916 also against the backdrop of war!
On May 3, 2017 Melissa J. Moore, Ph.D., Chief Scientific Officer for Moderna‘s mRNA Research Platform was elected to NAS “in recognition of their distinguished and continued achievements in original research.” [7] Moore was founding co-director of the RNA Therapeutics Institute (RTI).
Life Insurance premium 10% lower for patrons of homeopathy
In December of 1864 it was documented that a London Life Insurance Company began offering life insurance to Homeopathic patrons at a 10% discounted premium, because they were less likely to die than patrons who relied on Allopathic medicine. The insurance actuaries collected comparitive data that proved “the superiority of Homoeopathic treatment.” [1]
Though as early as 1855 it was reported in British Journal that two life insurance companies that offered “peculiar advantages to insurers who habitually employ homoeopathy for the cure of their maladies” [2]
The mortality under homeopathic treatment was lower, and sometimes substantially lower than for patients under the “regular” medical practice. Allopathic doctors were taught to ridicule and discount the practice of homeopathy as “quack” treatment, the truth was hidden from them.
Hidden Knowledge series – READ
U.S.13th Amendment passed into law, banning slavery
United States Republican lawmakers on December 6, 1865, passed the 13th Amendment banning slavery. “On January 31, 1865, the House of Representatives passed the proposed 13th amendment with a vote of 119-56. Abraham Lincoln did not live to see the amendment ratified. Republican President Lincoln was assassinated on April 14, 1865, and the amendment was not ratified until December 6, 1865.” [1]
Johns Hopkins establishes University and Hospital in his name
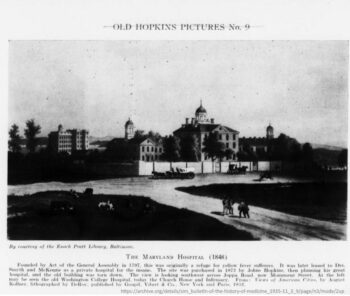 In 1867, Johns Hopkins, a Baltimore merchant and bachelor, arranged for the incorporation of The Johns Hopkins University and The Johns Hopkins Hospital, and for the appointment of a 12-member board of trustees for each. Hopkins died on Christmas Eve 1873, without seeing the end result, but left $7 million in his estate to be divided equally between the two institutions. It was, at the time, the largest philanthropic bequest in U.S. history. [1, 2]
In 1867, Johns Hopkins, a Baltimore merchant and bachelor, arranged for the incorporation of The Johns Hopkins University and The Johns Hopkins Hospital, and for the appointment of a 12-member board of trustees for each. Hopkins died on Christmas Eve 1873, without seeing the end result, but left $7 million in his estate to be divided equally between the two institutions. It was, at the time, the largest philanthropic bequest in U.S. history. [1, 2]
The land on which The Maryland Hospital stood, was purchased by Johns Hopkins in 1872, just before he died. [4]
It wasn’t until:
- 1889 The Johns Hopkins Hospital opened
- 1893 The Johns Hopkins University School of Medicine opened
“Johns Hopkins ushered in a new era marked by rigid entrance requirements for medical students, a vastly upgraded medical school curriculum with emphasis on the scientific method, the incorporation of bedside teaching and laboratory research as part of the instruction, and integration of the School of Medicine with the Hospital through joint appointments.” [3]
Hopkins recruited William H. Welch, William Osler, William S. Halsted and Howard Kelly – the so-called Big Four – by offering them rare and tempting research opportunities. The basic scientists and later the clinicians were free to do research by a full-time salary, and idea sold by Abraham Flexner, a departure from the tradition of employing part-time local practitioners to teach classes.
Johns Hopkins host many pandemic simulations (and more) including the coronavirus pandemic simulation “Event 201” in October 2019.
The American Public Health Association is formed
On April 18, 1872, following several years of planning by “a number of gentlemen” who were coworkers in the studies of “Preventive Medicine and in duties of public sanitary service”, they devised a plan to organise the formation of a public health association. The first conference was held September 12-13, 1872 where the formation of the organisation was unanimously adopted and called the American Public Health Association (APHA). The executive committee was elected September 13, 1872. [1, 2]
As written in their Constitution, their purpose was for “the advancement of sanitary science and the promotion of organizations and measures for the practical application of public hygiene.” Their members were to “be selected with special reference to their acknowledged interest in, or devotion to, sanitary studies and allied sciences, and to the practical applications of the same.”
In 1873 there were 2 epidemics were underway: cholera and yellow fever, and the recognition of Germ Theory of disease “had not yet become quite universal”. This same year they produced their first monthly publication of the Public Health Papers and Reports, which over 200 years has evolved into todays American Journal of Public Health.
From the outset they wrote ” State Medicine is not a chimera, and State interference would not be inconsistent with the most liberal and just government of a free people.” The proposed intervening to introduced “Preventive Medicine“!
The APHA spear-headed and influenced Public Health journals and policies right though to this today.
British Public Health societies take form
In the mid-to-late 1800 period great change was occuring within the areas of public health and sanitary reform. The UK passed the Public Health Act of 1875 on August 11, 1875, the following year the Sanitary Institute was established (1876) which was renamed the Royal Sanitary Institute in 1904. In 1955, the name was changed to Royal Society of Health. [1, 2]
“During its first fifty years, the (Royal) Sanitary Institute became the leading public health organization both in the United Kingdom and the rest of the world.”
Begining in 1856 the British Public Health Medical Society was established which in 1892 was incorporated as the British Institute of Public Health, and in 1897 when Queen Victoria became the patron, the name was changed to Royal Institute of Public Health. In 1937, it merged with the Institute of Hygiene which was established in 1903.
Then in October of 2008 the two institutes: the Royal Institute of Public Health (RIPH) and the Royal Society of Health (RSH) merged to be come the Royal Society for Public Health (RSPH) to be “an independent campaigning and educational charity dedicated to improving and protecting the health of people… both in the United Kingdom and around the world.” [3]
Still in operation today it he longest-established public health organisation in the United Kingdom. It is incorporated by Royal Charter said to be “completely independent of government and of any special interest.” [4]
Standardised dosage (Tabloid) lays foundation for modern (symptom focused) pharmacuitical industry
“Burroughs Wellcome & Co., founded in 1880, revolutionized the standardization of pharmaceuticals by introducing pre-measured doses in tablet form. While this innovation addressed the need for consistent dosing, the company’s products frequently lacked the clinical testing necessary to substantiate their claims.”
“The partnership of Silas Burroughs and Henry Wellcome further illustrates the complexity of this era. Co-founders of Burroughs Wellcome & Co. in London, they introduced “Tabloid” medicines, standardized doses of drugs in pill form. Their contributions to pharmaceutical standardization were significant, yet many of their early products were insufficiently tested, prioritizing marketability over rigorous scientific validation. This dual focus on innovation and profit laid the groundwork for the modern pharmaceutical industry while highlighting its enduring challenges.”
Their standardized dispensing and marketing strategies, along with that of Parke, Davis & Co. in the United States, “shaped public perception of medicine, fostering a culture in which immediate relief was often prioritized over addressing underlying causes of illness.” …”The emphasis on treating symptoms rather than root causes, a hallmark of patent medicines, became institutionalized in modern medical practice. ” …”By focusing on alleviating symptoms rather than addressing the root causes of illness, the [allopathic] system inadvertently creates a cycle of [highly profitable] dependency”. And so is born Polypharmacy. [1]
The parallels between 19th-century quackery and contemporary pharmaceutical practices are striking.
James Lyons-Weiler
[Placeholder data point]
Carnegie’s first public donation establishes first US laboratory – precedent for “community public health”
Sometime in 1884 Andrew Carnegie makes his first public donation in the amount of $50,000, to Bellevue Medical College in New York, the funding is to establish the Carnegie Laboratory which is America’s “first laboratory for teaching and investigation of bacteriology and pathology.” [1]
“The directors are Dr. Edward G. Janeway, who becomes a NYC health commissioner, and Dr. Frederick S. Dennis, who reports on the first investigations carried out at the laboratory on the action of micro-organisms on surgical wounds.”
Five years later in 1889, Bellevue hospital “physicians, Dr. Hermann Michael Biggs and Dr. Alfred Loomis, are the first to report that tuberculosis is a preventable disease. Dr. Biggs, the first crusader for community public health, writes that ‘no duty of society, acting through its government, is paramount to the obligation to attack the removable cause of disease.’ Dr. Biggs originates the first bacteriological laboratory in the US at Bellevue.” and develops bacteriological diagnostic techniques. In 1914 he becomes the NY State Medical Officer.
The world begins rapid electrification, and an era of new “electrical injuries”
On May 1, 1888 Nikola Tesla was granted US patent No. 382279 for the ELECTRO MAGNETIC MOTOR, alternating current (AC) system for the transmission of electrical power. This invention spurred on the electrification of cities around the world. [1, 2, 3]
In 1889 “quite suddenly” the world was being electrified on a scale that could scarcely have been conceived. So spectacular was the rapid growth of the electric railway in the US. [p79]
In November 2, 1889 published in The Medical Record is the topic of “Electrical Injuries” by Charles Dana:
With the development of new industries or inventions there occur new disorders or new factors in the production of disease and of injuries….We are now entering upon an era of tremendous activity in the practical application of electricity. Aside from the telegraph and telephone, electricity is becoming rapidly introduced as a method of lighting, heating, motor power, and locomotion….The means by which the electrical current does harm varies, naturally, with the form in which it is used…
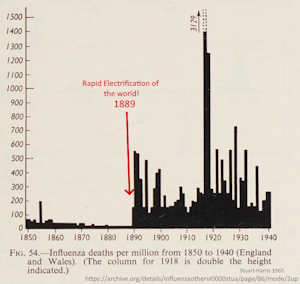 Influenza, the illness that had “received its name because its comings and goings were said to be governed by the ‘influence’ of the stars” and “whose descriptions had remained consistent for thousands of years” had “[s]uddenly and inexplicably…changed its character in 1889“, it would be for ever present around the world, reports Arthur Firstenberg [graph]
Influenza, the illness that had “received its name because its comings and goings were said to be governed by the ‘influence’ of the stars” and “whose descriptions had remained consistent for thousands of years” had “[s]uddenly and inexplicably…changed its character in 1889“, it would be for ever present around the world, reports Arthur Firstenberg [graph]
Pfeiffer’s bacillus discovered – said to be the causal agent of “influenza”.
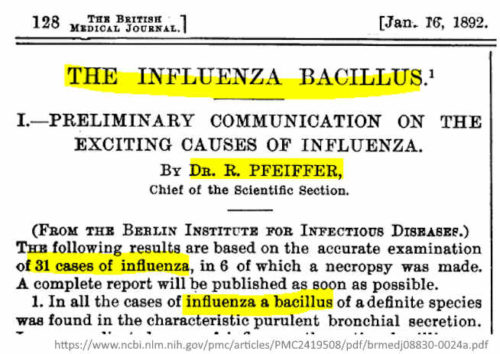 Following the examination of sputum from 31 patients who had died in 1889-90 flu epidemic, German bacteriologist Richard Pfeiffer discovered a new type of bacterium which “appear as tiny little rodlets”, it was reported in the British Medical Journal in January 1892. Pfeiffer was chief of the Scientific Section of the Berlin Institute for Infectious Diseases and a protégé of Robert Koch, as such people believed his findings. [1]
Following the examination of sputum from 31 patients who had died in 1889-90 flu epidemic, German bacteriologist Richard Pfeiffer discovered a new type of bacterium which “appear as tiny little rodlets”, it was reported in the British Medical Journal in January 1892. Pfeiffer was chief of the Scientific Section of the Berlin Institute for Infectious Diseases and a protégé of Robert Koch, as such people believed his findings. [1]
As the bacteria we found only in flu victims he considered himself “justified in pronouncing the bacilli …to be the exciting causes of influenza“. He named the bacterium Bacillus influenzae, but it was commonly referred to as Pfeiffer’s bacillus.
Pfeiffer’s bacillus was thought to be the causal agent for influenza during the early part if the 1918 pandemic, an “influenza vaccine” was even made, though dispute arose as the “bacilli” could not be isolated from all influenza cases or victims, and was found in asymptomatic persons. [3, 4, 5, 6]
Today the gram-negative coccobacillus is classified as Haemophilus influenzae in honour of it’s mistaken connection to influenza. [2] In 1995 H. influenzae is the first living organism (other than a virus) to have its genome fully sequenced. [7]
A new profession, Chiropractic, is born
On September 18, 1895 the founder of the chiropractic profession, Daniel David Palmer reportedly used spinal manipulation to restore the hearing of Harvey Lillard, a deaf janitor. As a result, Mr. Lillard claimed to “hear the wagons on the street,” something he could not do prior to receiving the treatment. This singular event is attributed to the genesis of a new profession called chiropractic, “one of the largest health care professions in the United States”. As is stated in a December 1997 report of the US Agency for Health Care Policy and Research (AHCPR) titled Chiropractic in the United States: Training, Practice, and Research. [1, 2, 3]
“Chiropractic is not a theraputical system. It deals exclusively with the cause of disease. It is a separate and distinct science based on giving a spinal adjustment for the cause of disease!”…”Germs are the cause of many diseases and healthy blood is the greatest germacide!”
D. D. Palmer allegedly stated circa 1906 in a debate with Dr Andrew Still, the founder of Osteopathy
“I maintain that chiropractic is a child of osteopathy!” shouted a biligerant Still
Osteopathy and Chiropractic were called “drugless” professions and along with Homeopathy were denegraded as “quackery” (and still are today), they were a big threats to the “Old School” medical establishement who employed coal-tar derived medicines, serums and surgery to treat disease. [4]
“Filterable virus” is first discovered
In 1898 Dmitri Ivanovski a Russian botanist, and Martinus Beijernick, a Dutch microbiologist and botanist, were independently given credit for the discovery of tobacco mosaic virus (TMV). The porcelain Chamberland filter apparatus use in the day excluded bacteria, and the resultant “poison” solution was said to contain “filterable virus“. Today this is deemed the begining of viruses as infectious agents smaller that bacteria. [1]